Lung Fibrosis Doctor in Mumbai
Idiopathic Pulmonary Fibrosis
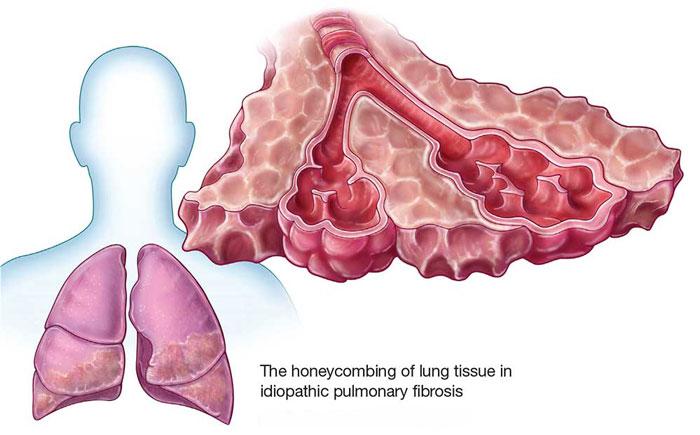
Pulmonary fibrosis (PF) describes a group of lung diseases in which thickening of the walls of the air sacs (called alveoli), caused by scarring, can result in cough,
shortness of breath, fatigue and low blood oxygen levels. Pulmonary fibrosis can be caused by an identifiable irritation to the lungs, but in many cases the cause is unknown. In cases when the cause of PF is unknown, the diagnosis is idiopathic pulmonary fibrosis (IPF). Idiopathic means there is no known cause at this time.
What Are The Symptoms of IPF?
When you have IPF, you may find yourself becoming more short of breath or having a dry cough. You may notice you cannot do your usual activities without shortness of breath. You may feel the need to slow down or stop and rest when walking, or it may become difficult for you to walk up inclines or climb stairs because of shortness of breath. Your healthcare provider may notice the oxygen levels in your blood drop when you walk. Lower than normal blood oxygen levels can cause high blood pressure in your lungs (called pulmonary hypertension).
Who Develops IPF?
- Most people with idiopathic pulmonary fibrosis develop symptoms of cough and shortness of breath between the ages of 50 and 70 years.
- IPF is not common under the age of 50 years. Historically, more men have been diagnosed with IPF than women, but IPF in women appears to be on the rise.
- Occasionally, IPF occurs in members of the same family. When this happens, the disease is called Familial Pulmonary Fibrosis.
How Does IPF Affect My Breathing?
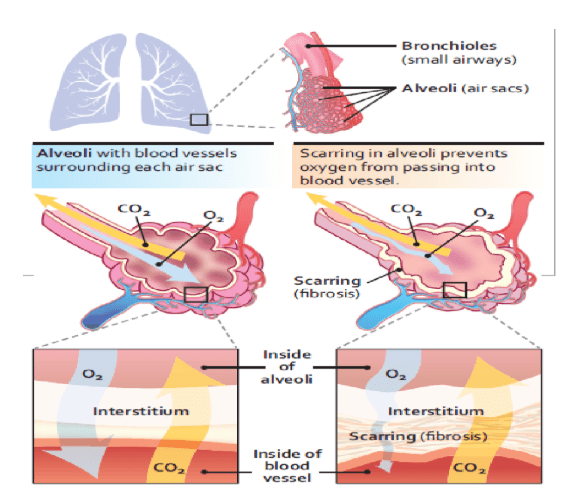
Air flows through your nose and mouth, deep into the lungs through large airways (bronchi) and small airways (bronchioles). These breathing tubes lead air into millions of tiny air sacs called alveoli. Within the walls of the air, sacs are a tissue called the interstitium. Much like a net, a collection of tiny blood vessels called capillaries surround each air sac.
The oxygen we breathe moves through the walls of the alveoli (including the interstitium) and into these surrounding capillaries, where the oxygen is picked up by red blood cells and carried to the heart. Carbon dioxide (CO2) moves in the opposite direction from O2 and is exhaled.
In IPF, the interstitium is thickened with scarring, making it difficult for oxygen to reach the capillaries. The scarring also makes the lungs “stiff” and difficult to inflate. Stiff lungs literally hold less air than normal lungs; that is, they have less filling capacity. This low lung capacity, along with the problem with oxygen passing through the walls of the air sacs, causes shortness of breath.
The amount of scarring can increase with time, making the lung even stiffer, further limiting its filling capacity, and limiting the ability of oxygen to pass through air sac walls. This scarring is generally not reversible.
How fast the scarring increases, varies from person to person. Some people may remain stable (with no decline in filling capacity) for several years, while for others, their breathing can worsen more rapidly.
How Does My Healthcare Provider Know I Have IPF?
Your healthcare provider may suspect you have IPF, based on your symptoms of a dry cough or shortness of breath. Abnormal breath sounds, called crackles can be heard by your healthcare provider when they have you take a deep breath. Crackles sound like Velcro® being pulled apart.
You or your healthcare provider may also notice that the ends of your fingers and/or toes have changed shape (called clubbing). These signs will likely result in you being referred to a lung specialist (pulmonologist). The pulmonologist will do a physical examination and may order several tests, such as a chest x-ray, breathing tests, or measurement of your blood oxygen level. Other tests that may be needed include blood tests, a high-resolution CAT scan (HRCT) of your chest, an echocardiogram (ultrasound or sonogram of the heart), and in some instances, a lung biopsy.
How Is IPF Treated?
As new treatments develop (or better ways to treat your symptoms become available), an IPF expert will know the best recommendations to make to you. Two new drugs, nintedanib, and pirfenidone, have been approved by the Food and Drug Administration (FDA) for the treatment of IPF. Prior to the approval of these two new drugs, corticosteroids (also called steroids) and immunosuppressant drugs were used to treat IPF, but they often provided no benefit and may have caused significant side effects.
Other therapies may be recommended to either treat your symptoms, or conditions that may develop as a result of having IPF. Such therapies include pulmonary rehabilitation, supplemental oxygen, and treatment of pulmonary hypertension.
What About A Lung Transplant For IPF?
Transplantation is major surgery and requires life-long treatment with drugs that overpower your immune system to prevent rejection of your transplanted lung. Not all patients with IPF can have a lung transplant. Ask your healthcare provider if you should be evaluated for a lung transplant. An evaluation for a lung transplant may take months, so your healthcare provider may begin discussing a transplant with you before your IPF gets severe.
Are There Special Things I Should Watch For?
Because you have a chronic lung disease, try to avoid situations where you can get a cold or the flu, and get your yearly flu vaccine. A small percentage of people with IPF develop what are called acute exacerbations. These occur when breathlessness from IPF suddenly becomes worse.
For more details and for consultation with Dr. Parthiv Shah who specialist lung fibrosis doctor in Mumbai.

Dr. Parthiv Shah
Best Pulmonologist in Mumbai
